Obsessive Compulsive And Related Disorder
The classification of Obsessive-Compulsive and Related Disorders (OCRDs) in the DSM-5 marks an important shift, as these disorders have moved from the Anxiety Disorders section to a distinct category due to their shared characteristics. Central to each disorder is obsessive preoccupation—whether it involves intrusive thoughts about contamination in OCD, worries about a physical flaw in Body Dysmorphic Disorder (BDD), or the compulsion to hoard items. To alleviate the anxiety of these obsessions, individuals perform repetitive behaviors or rituals, which can be mental actions like counting or physical acts such as checking, cleaning, or pulling hair. This grouping reflects common brain activity patterns and similar responses to treatments like SSRIs and Exposure and Response Prevention (ERP) therapy, emphasizing the cycle of distress that prompts these compulsive behaviors.
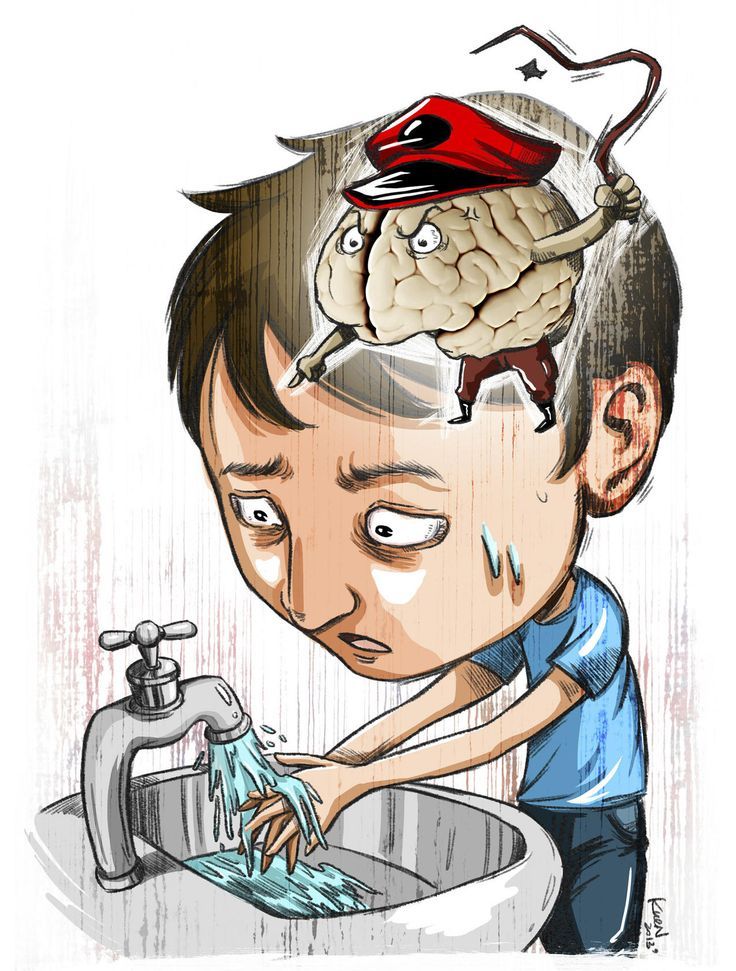
Obsessive compulsive Disorder
Obsessive-compulsive disorder (OCD) involves unwanted thoughts and fears, known as obsessions, that lead to repetitive behaviors called compulsions. These can interfere with your daily life and cause significant distress.
You may feel compelled to perform certain actions to relieve stress, but even attempting to ignore these thoughts usually doesn’t work. This creates a frustrating cycle of obsession and compulsion.
OCD often revolves around common themes, like a fear of germs. For example, you might wash your hands repeatedly until they become sore.
If you’re dealing with OCD, it’s normal to feel ashamed or frustrated. The good news is that effective treatment is available.
Symptoms:
- Fear of contamination or dirt.
- Doubting and having a hard time dealing with uncertainty.
- Needing things to be orderly and balanced.
- Aggressive or horrific thoughts about losing control and harming yourself or others.
- Unwanted thoughts, including aggression, or sexual or religious subjects.
Diagnostic Criteria:
A. Obsessions or Compulsions
- Presence of obsessions, compulsions, or both.
B. Obsessions
Obsessions are defined by:
- Recurrent and persistent thoughts, urges, or images that are intrusive and unwanted.
- The individual attempts to suppress, ignore, or neutralize the thoughts, urges, or images.
C. Compulsions
Compulsions are defined by:
- Repetitive behaviors (e.g., hand washing, checking) or mental acts (e.g., counting, praying) that the individual feels driven to perform.
- The behaviors or mental acts are aimed at preventing or reducing anxiety or distress.
D. Time-Consuming or Interfering
- The obsessions or compulsions are time-consuming (taking more than 1 hour per day) or cause clinically significant distress or impairment in social, occupational, or other important areas of functioning.
Body Dysmorphic Disorder
Body Dysmorphic Disorder (BDD) is a serious mental health issue where individuals obsess over perceived flaws in their appearance, often minor or unnoticed by others. This isn’t just normal self-consciousness; it can be very distressing and take up hours each day, leading to behaviors like constant mirror checking or seeking reassurance. BDD can affect anyone, typically starting in the teenage years or early adulthood, and it concerns both men and women, sometimes focusing on body image issues like muscle size in men. It’s important to note that BDD isn’t about vanity; it stems from deep feelings of inadequacy and can lead to significant emotional pain and social withdrawal. Professional help, such as Cognitive Behavioral Therapy (CBT) and sometimes medication, is often needed for treatment.
Symptoms:
- worry a lot about a specific area of your body (particularly your face)
- spend a lot of time comparing your looks with other people’s
- look at yourself in mirrors a lot or avoid mirrors altogether
- go to a lot of effort to conceal flaws – for example, by spending a long time combing your hair, applying make-up or choosing clothes
- pick at your skin to make it “smooth”
Diagnostic Criteria:
A. Preoccupation with Appearance
- Preoccupation with one or more perceived defects or flaws in physical appearance that are not observable or appear slight to others.
B. Repetitive Behaviors or Mental Acts
- At some point during the course of the disorder, the individual has performed repetitive behaviors (e.g., mirror checking, excessive grooming) or mental acts (e.g., comparing oneself unfavorably to others) in response to the appearance concerns.
C. Significant Distress or Impairment
- The preoccupation causes clinically significant distress or impairment in social, occupational, or other important areas of functioning.
Hoarding Disorder
Hoarding disorder involves difficulty in discarding possessions because you feel the need to keep them. This can lead to distress at the thought of getting rid of items, resulting in the accumulation of many belongings, regardless of their true value.
As hoarding increases, living spaces can become extremely cramped, with only narrow paths through piles of clutter. Surfaces like countertops, sinks, and desks may be overwhelmed with stuff, making it hard to use certain areas, like cooking in the kitchen. When indoor space runs out, clutter can spread to garages, vehicles, and yards.
Hoarding can vary in severity; sometimes it has little impact on daily life, while at other times, it can severely disrupt functioning. Individuals with this disorder often don’t recognize it as a problem, making treatment participation difficult. However, intensive therapy can help change beliefs and behaviors, leading to a safer and more enjoyable life.
Symptoms:
Hoarding disorder symptoms include:
- Keeping too many unnecessary items without enough space.
- Difficulty getting rid of things, no matter their value.
- An emotional attachment to items, causing distress at the thought of disposal.
- Cluttered spaces that prevent you from using rooms properly.
- Trouble making decisions and organizing.
Consequences of hoarding can lead to:
- Disorganized piles of items like clothes, papers, and sentimental belongings.
- Areas of your home becoming unusable, like not being able to sleep in your bed.
- Accumulation of food or trash creating unsanitary conditions.
- Stress and challenges in keeping yourself, others, and pets safe.
- Strained relationships due to clutter conflicts.
- Social withdrawal and job issues.
- Losing important items in the mess.
You may save items because:
- You think they are special or may be needed later.
- They remind you of happy memories or loved ones.
- You find comfort in having many belongings.
- You want to avoid wasting anything.
Diagnostic Criteria;
A. Persistent Difficulty Discarding Possessions
- Persistent difficulty discarding or parting with possessions, regardless of their actual value.
B. Strong Urge to Save Items
- The difficulty is due to a strong urge to save the items and/or distress associated with discarding them.
C. Accumulation of Possessions
- The difficulty discarding possessions results in the accumulation of possessions that congest and clutter active living areas.
D. Significant Distress or Impairment
- The hoarding causes clinically significant distress or impairment in social, occupational, or other important areas of functioning.